Preamble
Brandon Blue - Roundtable on Black in cancer research and oncology
Saying hello and good morning, afternoon, evening, wherever everyone is joining from. My name is Kathryn Mcginnis. I'm an editor at the Cancer Team in Nature Communications and myself and my colleague, Lisa, who is joining from Nature Cancer. And we're delighted to welcome you to this Roundtable Discussion on Black and CANCER RESEARCH and Oncology.
What we're really hoping for today is to have a fruitful and thought-provoking Discussion with our very eminent speakers and also to welcome questions and comments from you as our audience. We're very aware that our audience is partly editorial staff from Springer Nature and also people from further afield.
So just some very quick housekeeping to start. This meeting is being recorded and it will be made available to all participants after the session. You will be able to submit questions during the talk using the chat function which should be on screen. And we've also prepared some questions that have come from the cancer community already within Springer Nature.
But first of all, we'd like to start introducing you to our speakers for this session. So without further ado, I'd like to introduce our first speaker who is Dr. Brandon Blu. So Brandon is an oncologist at the Moffit Cancer Centre and is very kindly joining us from there and he's working to increase inclusion within clinical research.
So, Brandon, if it's all right, I'll hand over to you. Thank you so much. I'm so happy to be here. I appreciate everyone for this time period and I am going to share my screen so I can talk to everyone about kind of what I do in sunny Tampa Florida here in the United States and how we can hopefully have a very wonderful conversation today. Eight, we go, all right, perfect. So hopefully, folks are seeing my screen and we are able to get started. So, you know, I am a doctor who basically sees Blood and bone marrow cancers.
One of the specialties we focus on is stem cell transplants, along with a newer therapy called car T cell or chimeric antigen t-cell receptor therapy. This concept has been around for decades, with the idea of utilizing the immune system to combat cancer. Our immune system plays a vital role in fighting off various illnesses such as bacteria, COVID, and pneumonia. However, through extensive research, we have discovered a method to utilize the T cells' potential to fight against cancer instead.
And so, what happened is that we utilize different domains to deceive the immune system into believing it is combating the latest strain or variant of COVID. However, in reality, it is targeting specific cell markers that are commonly found on certain malignant cells. Fortunately, we are able to modify the types of malignant cells that we can manipulate the immune system into attacking. As a result, this therapy can be applied to various types of cancer.
You can see that once the immune system is activated, these T cells really go to work. And honestly, that's what T cells do - they know that they should be killing. This is a very novel concept because T cells have always killed things. However, now we're just changing that target and allowing the immune system to be activated in a way that it fights off cancer cells.
Right now, this is really on the precipice of where most blood and bone marrow cancers are basically being treated. This is a way that is innate and almost a natural way to get rid of cancer or to get rid of extra cells that shouldn't necessarily be there in the body.
And so, in this particular case, our goal is to refine and improve our systems and methods. This is an area of research that I focus on, as we are aware that cells communicate through different signaling pathways. Our aim is to ensure that these cells communicate with each other in a way that leads to sustained killing of abnormal cells. To illustrate, let's consider multiple Myeloma, a type of cancer that is currently being studied and developed. Unfortunately, it is not currently curable and mainly affects plasma cells in the bone marrow.
Our objective is to determine if CAR T cells, which are infused into the body, can continue to signal and communicate with each other. We want these cells to remain active long after they are introduced, so they can engage in immune surveillance and eliminate abnormal plasma cells. This information is crucial for those who seek a detailed understanding of the mechanisms involved. It is important to note that the immune system is typically triggered by certain cytokines in the body, which indicate the presence of a problem. For most individuals, this activation occurs in response to an infection.
In this particular case, we are utilizing the same mechanism but with a different approach when it comes to cancer. It is important to understand that the co-stimulatory domain has shown promising outcomes across various types of cancer.
And again, in this particular case, we're primarily focusing on blood and bone marrow cancers. However, research in this field is rapidly expanding to encompass various types of cancer. Currently, the standard treatment for many patients is chemotherapy, which has traditionally been offered.
And we can see that by using this kind of salvage treatment and a way of using to activate the T cells is really something that's important and actually may be even better compared to standard chemotherapy treatments.
However, one of the things that we can see is that over time, the type of cancers that were available have changed.
So, for example, it started out typically in what we call lymphoma and leukemia. And most recently, we've had approvals, at least here in the United States, from the FDA, for two CAR-T cell therapies for multiple myeloma. The headlines are showing that this is the direction all blood and bone marrow cancers are heading, and we're very excited about it.
However, one thing we wanted to address, especially for this audience, is that as these new therapies emerge, we must ensure that no group of people is left behind.
And so, what we were able to see is that the access to these new therapies for people unfortunately created an issue, as it was not standardized across the board. Not everyone who had this new emerging novel way of treating cancer had access to it. Unfortunately, this is something we are trying to change.
To evaluate this, one of the things we did that we are very proud of is sending questionnaires to some oncologists here in the State of Florida. We asked them if they send people to Cart, and if not, why not. Through our research, we found that doctors who were less likely to understand Cart and how to take care of Cart were also less likely to send people for it.
It is important for people to know that once they come to us for Cart, they don't stay as a Cart patient. They do go back to their community, and their local doctor is typically able to take care of them.
So, I can understand how being a local oncologist, if you are not experienced in providing care for patients after undergoing complex therapy, it might make you feel hesitant to make referrals. Unfortunately, certain communities were impacted more by this lack of access. Specifically, minority communities did not have the means to reach these large academic centers independently. It is crucial for us to acknowledge this fact in terms of clinical trials as well.
Those are the things that we are trying to bring to the community to ensure that people not only have access to approved therapies but also increase our clinical trial enrollment for minorities. As the clinical trials continue to evolve and make these treatments more widely available, it is important to prioritize diversity in our research. This will help ensure that all communities have equal opportunities to benefit from these advancements in medical science
We would like to express our gratitude to everyone for their time. However, I would like to mention that we have conducted a new research study that we intend to present at a national conference. This study addresses not only the issue of access, but also focuses on individuals with the same type of cancer. It has revealed that the time from their diagnosis to receiving a referral for treatment varies between Black and Hispanic patients.
And so, those are things that we are trying to improve. Those are some things that we are doing in our research, and hopefully, we will have a lively discussion today. I thank you for your time again. I am Doctor Brandon Blu from Moffit CANCER CENTER in Tampa, Florida. Thank you.
Thank you, Brendan. That was great. And I think it already gives us a lot of opportunity to discuss later. So if you have any questions, remember them for afterwards. But now, it is my great pleasure to introduce our second speaker, who is Doctor Kilen Ashad Bishop. She is a biomedical scientist who obtained her PhD from the University of Miami in 2019. She co-founded Stem No R, which is a research and wellness community for black women in Stem. Kilen, thank you so much for joining us today.
Yeah. Thank you for the invitation. So, I am going to share a few slides. Alright. So, I will be talking a little bit today. I will talk about some more at the end, but I will start with talking a little bit about my work in socioenvironmental determinants of cancer disparities.
Kilan Ashad-Bishop - Socioenvironmental Determinants of Cancer Disparities
First, I don't believe in giving any scientific talk without contextualizing who I am and what I care about. I love being outside. I love my cat babies. I love bringing outdoors indoors via my plant babies and favorite food french fries.
Now, when it comes to science, my training is diverse. I started in Basic Biology, molecular Cancer Biology for my PhD and eventually transitioned to population science via two postdoctoral fellowships. One fellowship focused on education and human development, while the other centered around cancer disparities and equity.
I have now focused my attention on what I consider to be my niche, which is climate justice and cancer disparities. This is because when we consider the populations that are most affected by the unequal consequences of climate change, we find that they are more likely to experience increased exposure to carcinogens due to their proximity to power plants or roadways. Additionally, these populations are also more likely to suffer the consequences of extreme weather events that are related to climate change.
We can observe that certain populations face increased exposures and neighborhood-level sensitivity due to historical disinvestment and racial segregation. These populations also have decreased adaptive capacity, such as lower income, limited formal education, and lack of access to transportation, which hinders their ability to cope with concentrated disadvantage. It is worth noting that these same populations also experience disparities in cancer outcomes. Therefore, they are not only at the forefront of climate change but also suffer from unequal cancer outcomes.
My work focuses on the intersection of these domains, and I will discuss one study today that examines how socio-demographic indicators of climate vulnerability are associated with cancer screening participation. To accomplish this, we utilized a machine learning technique to characterize the socio-demographic indicators of climate vulnerability using an index.
Miami-Dade County has organized its tracks into clusters based on social vulnerability. These clusters can be seen as neighborhoods, characterized by their climate vulnerability profiles. Interestingly, we observed that these clusters tend to concentrate in specific areas of Miami-Dade County.
But also, it is important to note that these profiles of climate vulnerability are directly linked to differences in cancer screening participation. These neighborhoods have a high concentration of populations who are more likely to suffer from climate exposures that negatively impact their health. Additionally, these neighborhoods are often vulnerable to these threats systematically.
Ideally, we would expect these populations to have higher-than-average participation in cancer screening in order to prevent the emergence of future hotspots of cancer incidents and even mortality. However, the reality is quite the opposite. This emphasizes the significant amount of work that still needs to be done.
This work highlights the importance of considering co-beneficial interventions that address the social context and the world around us in order to improve outcomes in behavioral risk factors, such as cancer screening. It is crucial that we think more intentionally about these interventions to bring about positive change.
When conducting Health Disparities Research, it is crucial to consider the changing world we live in. We are witnessing an increase in the frequency and severity of climate-driven extreme weather events, along with record-breaking extreme heat and devastating wildfires that are becoming increasingly difficult to contain. It is important to remain vigilant and acknowledge how these disasters can further distance certain individuals from receiving necessary care. Additionally, it is worth studying how certain populations may be more susceptible to the biological risk factors that arise as a result of these disasters.
In addition to my scientific pursuits, I also curate an identity-based affinity space called STEMNoire. STEMNoire is a research and wellness community specifically designed for black women in science, technology, engineering, and math. Our community is global and offers year-round programming to support and empower black women in these fields.
Our signature program is the seminar conference held each summer. We received feedback from social media regarding our first virtual seminar conference in 2021. We also held another virtual conference in 2022. Last year, we brought our communities together in person in San Juan, Puerto Rico. The consistent message we hear from our community is that their current academic and research spaces do not provide opportunities to incorporate their identity into their work. They often feel unseen and there is no room for their personal experiences alongside their scientific pursuits. We take pride in curating a space where individuals do not have to choose between their race, gender, or profession. Instead, they can embrace all aspects of their identity. If you know a Black woman in STEM who may benefit from connecting with our community, please direct them to our website or social media. We are always looking to expand our community and provide support. Additionally, I would like to acknowledge the Sylvester Comprehensive Cancer Center and the 2 32 program for their contributions to this work. The leading edge community is another affinity-based space for women in academia. Lastly, I am currently affiliated with the American Cancer Society.
Thank you so much. It's great to talk about cancer research in a holistic sense. Cancer is never seen in isolation, so it's important to have discussions about climate change and identity alongside that. I hope we can get some questions related to those topics.
In the meantime, I know some participants have been experiencing connection issues. This meeting will be recorded, so if anyone is having trouble with the connection, they can watch the recording later. We are currently in contact with the platform's support team to see if there is anything we can do to address the issues.
Now, I would like to introduce you to a blog. She is a radiation oncologist at Well Cornell Medicine, specializing in gynecological and breast malignancies. She focuses on improving the patient experience for those with these conditions. You might also know her as one of the onc dos who host a wonderful podcast. Their podcast highlights the stories of Black cancer oncologists and survivors, amplifying their voices.
Thank you for the wonderful introduction. Unfortunately, my better half is at a conference, so I am the only one here today. However, I am still very excited to speak to all of you about a topic that is important to me and I hope will become important to all of you.
Onyinye Balogun - The Black Patient Experience in Endometrial Cancer
The Black patient experience in Endometrial Cancer is the focus of this text. I will begin by providing my disclosures. Today, my goal is to discuss and review the statistics related to Endometrial Cancer, also known as Uterine Cancer. Endometrial Cancer specifically pertains to the lining of the uterus and is the most prevalent form of cancer that originates in the uterus.
So I just wanted to clarify that because you might see those terms used interchangeably. I also want to, of course, talk about the inequities when it comes to black individuals and endometrial cancer and discuss how genomics may help us tackle those inequities.
When we look at endometrial cancer, it is the most common gynecologic malignancy in the United States. Similarly, in most developed countries, it is also the most common.
In low and middle-income countries, cervical cancer is not the most common type of cancer. However, recent statistics and discussions with my colleagues indicate that it is increasing in prevalence. Therefore, addressing this issue is crucial.
Initially, cervical cancer may seem to have a relatively high survival rate compared to other cancers, with a five-year survival rate of 81%. However, there is a concerning trend of rising incidents and mortality rates for endometrial cancer. This data is derived from the annual cancer report to the nation, which reveals that uterine cancer is not only increasing in incidents but also has the highest mortality rate among all cancers.
And that's really a problem. As we see our population aging and people living longer, we are grappling with the challenges of disease. Unfortunately, we know that there are disparities in endometrial cancer. This has been discussed in numerous articles, and I would recommend referring to the AACR cancer disparities progress reports, which I have had the pleasure of contributing to. Initially, this was a problem that we weren't giving much attention to, but I am relieved to see that we are now sounding the alarm because it is a matter of great concern.
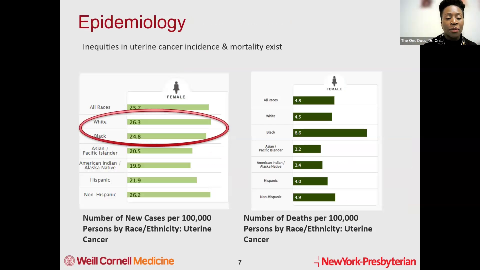
When discussing cancer disparities, it is important to clarify that I am referring to differences in incidents, prevalence, mortality, and survival rates. Specifically, I am focusing on the disparities between black women and women of European ancestry. Despite similar incidents of Uterine Cancer among white and black women in the United States, black women have twice the mortality rates. To further explore this issue, I conducted a study for my master's thesis in New York City. This microcosm allowed me to examine if the situation in the city reflects the national trend. The findings revealed that over a span of approximately 20 years, black women in New York City surpassed white women in terms of the incidence of Uterine Cancer.
The rate at which it happened was quite alarming and statistically significant. Additionally, in terms of mortality, black women experienced a sharper rise in deaths over the same period of time.
And so, we are currently attempting to determine the cause behind this occurrence. Several studies have been conducted, one of which is particularly noteworthy - the study conducted by Doctor Felix. The purpose of this study was to explore the disparities in outcomes based on race and ethnicity within the context of the gog 2 10.
Doctor Felix's findings revealed that black women are more prone to experiencing recurrence of the disease compared to non-Hispanic white women. Furthermore, they are also at a higher risk of mortality as a result of this illness.
And there are a number of different reasons. But one of the key things that she drew out from this study is that these findings, even if we control for socioeconomic status or the same treatment, the treatment that they were supposed to receive because we know that can be an issue, right? In terms of inequities, sometimes black women do not get what the standard of care should be. And that is an issue in and of itself.
But what struck me about this paper is that despite even if they get the right treatment, even if they are well enough to do that, they can access treatment in a timely manner, they have worse outcomes. So one of the questions that came up for me is why, why, why is this the case?
This is a figure from that cancer disparities report I mentioned earlier, showing that there are many different factors that can contribute to cancer inequities. One of the ones that has most intrigued us are the biological factors. And this has led us to projects like the Cancer Genome Atlas as well as PROJECTGENIE, where we're trying to understand what the biological underpinnings of these inequities are.
And now, it is important to note that our focus should not solely be on biological inequities or biological mechanisms. I strongly believe, as Doctor Bishop so eloquently demonstrated, that it is the interaction between our internal biology, the surrounding environment, and our internal environment that plays a significant role. I want to emphasize this point to avoid any potential disagreement. All aspects, including our biology and both internal and external environment, interact to contribute to these disparities. Despite initiatives like the Cancer Genome Atlas and the Project genie from AC R, it is evident that there is a significant lack of diversity in these genomic databases. Considering the US population, approximately 12% are Black individuals and 6% are Asian individuals. However, it is concerning that, even after more than two decades of tumor profiling through these studies, over 75% of the samples included in these genomic studies come from people of European ancestry.
And so, that just basically reflects who we enroll in clinical trials. I'm sure many of you have heard the conversations about the lack of representation from different minority backgrounds in clinical trials. This issue also affects the genomic studies we conduct to understand cancer, as we don't enroll enough individuals.
For instance, with the TCGA, it is evident that over 75% of their participants are of European ancestry. This trend is similarly observed with the Project genie. However, it is crucial to enroll individuals from diverse backgrounds because there are clear differences that need to be accounted for.
This is the Cancer Genome Atlas study for Uterine Cancers. It reveals that Uterine Cancers can be classified into four different classes based on their genomic profile. The Subtype of the cancer has an impact on disease recurrence. On the right-hand side, you can see that the Subtype called pole mutant has the best outcomes, followed by the Subtype called M si high. The Copy Number low Subtype comes next, and finally, the Copy Number high Subtype. It is known that black women are more likely to fall into the Copy Number high Subtype due to their higher prevalence of P53 and her two mutations.
To gain a better understanding of the underlying biological reasons for these disparities, I partnered with Dr. X from North Well Health and Cold Spring Harbor. Together, we developed a proposal to the New York Genome Center to study the mechanisms of ENDOMETRIAL CANCER DISPARITIES specifically in black women.
And so, this is part of a project called the Poly Ethnic 1000, in which I also have a role as a cancer and inequity scholar. We are funding about seven different projects looking at eight different tumors through the Poly Ethnic 1000. Our focus is on enrolling populations from minority backgrounds to understand the spectrum of bio changes that may lead to cancer inequities.
I am particularly proud of our project because I work at Brooklyn Methodist, a community hospital that is not typically known for this type of research. However, we have created the necessary infrastructure to carry out this project. We recognize that individuals from minority backgrounds often seek treatment at community hospitals rather than academic centers.
Here is our workflow: we obtain informed consent from participants, collect blood and uterine tumor samples during surgery, and send them for DNA and RNA sequencing. Additionally, we aim to grow organoids, which involve taking a piece of the tumor.
And we frequently try to replicate it in mouse models in order to test new drugs and better understand how tumors grow and what causes them to die off. Our main aims were to establish a biobank and define the unique biologic features of Endometrial Cancer in women of African ancestry. We also wanted to examine the mechanisms of disparity. I am pleased to announce that we have successfully collected about 100 samples and will release a report by the end of the year or early next year. As Doctor Bishop mentioned, I was born in Nigeria and have maintained relationships there. I am passionate about addressing disparities both domestically and globally. Another initiative we have started is called Aja Africa, the Diaspora rising against Endometrial Cancer. We have collaborated with experts such as Doctor Lisa Newman and Doctor Melissa Davis, who have been studying breast cancer internationally for many years. I was fortunate to approach them and ask if we could utilize their networks to study Endometrial Cancer, specifically on the African continent.
Because if we want to truly comprehend the impact of African ancestry on Endometrial Cancer, it is crucial to take a broader perspective. Therefore, I am thrilled to collaborate with various individuals and institutions. We have recently submitted a research proposal, and now we eagerly await updates within the next year.
In conclusion, it is evident that black women bear an unjustifiable burden of Endometrial Cancer. Regrettably, they are underrepresented in clinical research. However, we are actively making significant strides to include them, aiming to gain a better understanding of the issue and develop solutions for these disparities. Thank you for your attention.
Thank you for this enlightening presentation. It has made us all aware of the significant disparities in genomic research. I am eager to discuss how we can address this issue, particularly within our editorial community.
Before we delve into that, I would like to introduce Dr. Runcie Chidebe, the Executive Director of Project Pink Blue. This organization in Nigeria is dedicated to fighting cancer and aims to collaborate with the government, non-profit organizations, and the private sector to provide support for cancer patients.
Now, I will hand the stage over to Runcie. Thank you for being here. Please feel free to share your screen and begin your presentation. Let's ensure everyone is ready.
Runcie C. W. Chidebe - If there is no data, create it: Project PINKBLUE's story of Oncology Research & Practice
Yeah, thank you so much. My name is Ron CCW Chidebe. I'm the Executive Director of Project Ping Blue. I'm also a Patient Advocate and an Oncology Researcher. These roles represent my disclosures.
So, today, I want to talk about and share our story. I strongly believe that in any situation where there is a lack of data, our approach should be to proactively create the necessary data.
We often hear the argument that there is a lack of data and infrastructure to generate this data. However, I have a different perspective - if there is a dearth of data, we should strive to create it. Allow me to provide a few examples of the initiatives we have undertaken and are currently undertaking in Nigeria. These examples serve to demonstrate what is possible and to highlight the potential for Nigeria, Africa, and numerous other low and middle-income countries to spearhead advancements in cancer control. This includes addressing the incidence and mortality rates, conducting clinical research, and various other aspects related to cancer control.
So Nigeria is one of the underserved regions of the world, and the country is a major contributor to cancer burden in the African continent. As some of you may be aware, in Nigeria, over 120,000 people are diagnosed with cancer every single year, and over 70,000 people die from this disease. This high mortality rate is due to the fact that 70% of people diagnosed with cancer are diagnosed at a very late stage, typically stage three or stage four.
Late diagnosis of cancer is a widespread issue in Africa and many low and middle-income countries. Scholars, policymakers, and stakeholders often refer to this problem using the catchphrase "delayed diagnosis". It is impossible to attend a conference anywhere in the world discussing Africa without hearing this term. Unfortunately, in many cases, people use the concept of late diagnosis to blame the cancer patients in these regions.
I want to emphasize that most cancer patients are not responsible for their late diagnosis. The weak cancer health system, including a lack of national cancer screening, limited diagnosis and treatment capacity, and other factors, are to blame for the delayed detection. Instead of placing blame on the patients, we should focus on addressing the shortcomings of the health system.
So, as I mentioned earlier, I work with Project Ping Blue. Our main focus at Project Plue is addressing various issues, particularly the detection of cancer. We have been actively reaching out to millions of Nigerians and individuals across Africa. Our initiatives involve training doctors, pharmacists, nurses, and anthropologists. Additionally, we conduct numerous programs throughout the country.
So, the first example is about a significant issue: deciding where to seek medical help when one has cancer or experiences symptoms. To address this problem, we developed a Patient Navigation program. This initiative involved training nurses and establishing a comprehensive system that guides individuals to appropriate healthcare facilities when necessary. The aim was to assist people in knowing the best options available to them.
If there was a need for diagnosis or treatment, we were there to provide assistance. We are incredibly grateful for the generous grant of fifty-seven $1000, which was awarded to us by the Union for International Cancer Control and Pfizer Oncology. This grant allowed us to successfully run this project in 2016. As a result, we have been able to highlight the significant impact of this project in various research publications.
This was a Project, a Palliative Care Project that we did with UT MD Anderson. And over here, over here is the patient navigation training that we also had as part of this program to ensure that women are finding the, you know, where they need to do Diagnosis and treatment.
Example two is that we've seen several situations whereby people say that men are not interested in cancer. So Nigeria has a unique form of Cancer incidence and mortality in relation to Other countries.
You know, Lung, gumbo cancers are the leading cause of cancer deaths in countries like the UK, for instance. However, in Nigeria, cancers such as breast cancer, cervical cancer, and other infectious diseases related to cancer, like hepatitis and liver cancer, are on the rise. On the other hand, prostate cancer is a greatly neglected cancer in terms of awareness and support. Many men have been dying from prostate cancer, yet their plight remains unnoticed. The unanswered questions that persist are why men seldom seek diagnosis and fail to take proper care of themselves. It seems that men are generally disinterested in cancer.
So, what we did was launch the Menon Blue Project. This project focused on prostate cancer intervention and was funded by a foundation based in Lagos. Our goal was to provide screening to 1661 men from diverse ethnic groups and living in different cities across Nigeria. We offered these men a free Prostate Specific Antigen (PSA) test. Additionally, we conducted research to assess their knowledge about prostate cancer and to understand the correlation between their PSA levels and their willingness to pay for screening.
Would they be willing to pay for screening in the future and all the rest of them? The interesting finding for this research is that, aside from being one of the first and largest studies in prostate cancer in Nigeria, which included education, screening, and follow-up. The interesting thing was that most men really, really appreciated this intervention because we used that opportunity to follow these men for almost six months.
Now, the third example is: can I receive optimal treatment if I have any form of cancer? Let's consider this situation. Cancer is currently one of the most glaring examples of global health inequality, as survival rates and mortality rates vary significantly among continents and countries. For instance, in high-income countries, the survival rate has almost reached 80%. However, in Africa, it can be as low as 40% to 20%. This discrepancy can be attributed to several factors, such as inadequate training of cancer experts and limited access to cancer treatment. Additionally, misdiagnosis and lack of access to necessary medications further contribute to the problem. Consequently, there is a growing tendency to blame cancer professionals, particularly oncologists, for not delivering optimal care. However, it is important to acknowledge that one cannot provide what they do not possess. If our cancer specialists lack proper training, they are unable to provide the necessary care. In response to this challenge, Project Plue has collaborated with the US Department of State and the US Embassy in Abuja to establish a comprehensive specialist program. Since 2018, we have been inviting two cancer experts from the US to visit Nigeria for at least two weeks and provide training to Nigerian professionals.
In 2018, we hired two medical oncologists and in 2021, we brought in two US oncology professors specialized in pharmacy. Additionally, last year we conducted a zoom session for pathologists. The remarkable aspect of this project is that it aims to equip cancer professionals with the necessary skills within their own working environment, utilizing the available infrastructure. This is in contrast to the common practice of sending specialists from Nigeria abroad for training, which, although beneficial, often results in their inability to practice upon returning due to the lack of similar infrastructure in their home country. Moreover, we have also shared our approach and methods to enable the scientific community and individuals in other countries to learn from and replicate our success.
The issue at hand is the lack of patient voices in research, particularly in low and middle-income countries like Nigeria. In these countries, people often do not believe that many individuals survive cancer because they rarely see cancer patients coming forward. This misconception is perpetuated by the images found when searching for cancer survivors in Africa on Google, which predominantly depict individuals who appear to be on the brink of death. However, these images only represent a specific phase of cancer survival, and it is crucial to promote a more comprehensive understanding.
To address this, in 2017, we established the Abuja Breast Cancer Support Group, which is the first of its kind in Abuja. The purpose of this group is to foster connections among men and women impacted by breast cancer, providing support and a platform for sharing stories. This initiative has been empowering for both men and women, as they learn from each other's experiences.
In 2019, the men within the support group began questioning why our focus was solely on breast cancer patients. They raised a valid point, highlighting the need to support women with prostate cancer as well. As a result, we expanded the group to include all individuals impacted by cancer in Nigeria, forming a network under one umbrella organization. This network serves as a platform for advocacy, care provision, and support for anyone affected by cancer, not just breast cancer.
This expansion has allowed us to become a national advocate for cancer patients, with over 200 individuals willing to uplift and be a voice for other cancer patients, particularly women. Our goal is to increase awareness and understanding of cancer survival, showcasing individuals like Gloria, AA, and countless other women who have successfully
Now, I just wanted to share some of the key information that we've seen. This is from some of the ongoing research. And this is what a patient said.
"It's been a very painful journey. Most especially when the vein collapses, I suffer a lot. Maybe it's because I'm big and need about nine pricks for chemotherapy. Nine full pricks. Every part of my hands is on the line before I take chemotherapy because I know I'm going to feel pain. I am going to feel another pain and still the result is not successful. In fact, it got to the point of using my leg and it's still difficult. I would say to the doctor, I would say the doctors are not patients, they are not well trained. The impatient level can lead you to develop cancer on its own."
I will share some background information to provide context for the following quotes. In Nigeria, the use of totally implantable venous access parts is not popular. Instead, people still use the normal intravenous (IV) method. This has a significant impact on women, especially breast cancer patients, who experience a great deal of pain as they have to go through multiple procedures just to receive one chemotherapy treatment.
Now, let me share another quote from an elderly woman. She said that you don't wish pain upon your enemy. I personally experienced pain during my chemotherapy period, to the point where I even attempted suicide. The pain is indescribable and difficult to explain. It's hard to pinpoint where exactly it is coming from - whether it's in your stomach, your head, or your entire body. This pain is beyond words.
So, the goal of my presentation today is to encourage all of you to become advocates for Black people. When you advocate for Black people who are impacted by cancer, you are also advocating for yourself. A cancer patient in Lagos is no different from a cancer patient in Lisbon, London, Dallas, or Melbourne.
What differentiates these cancer patients is actually the treatment that they have access to. I believe that all forms of inequalities, injustice, and lack of access to healthcare are the most severe.
One striking example of this is that more than 90 percent of all cancer patients participating in prostate cancer clinical trials are white men.
You know, even when we know that Black men represent 20% of prostate cancer diagnoses, there is a large inequity in the distribution of clinical trials and access to cancer treatment.
Globally, many metastatic breast cancer patients in low and middle-income countries face the significant challenge of not having access to clinical trials and essential medicines. A striking example of this issue can be seen in Africa, where there are currently only a few, if any, open oncology clinical trials available throughout the entire continent.
So, just to give you an example, if some of us are already aware of clinical trials, for instance, in 2019, a medication known as AAA was approved by the FDA as a treatment for patients with breast cancer. A glance at this pie chart shows the percentage of patients recruited by race. It is clear that only 8% of the patients recruited were Black. Additionally, there were about 376 patients in total. Having access to clinical trials has many benefits for patients, as it provides potential opportunities to prolong and improve the lives of women with breast cancer.
Another example is a medication used for metastatic cervical cancer, which affects many Africans and Black individuals.
In low and middle-income countries, particularly in Africa, the burden of cervical cancer poses the greatest risk. However, there is hope in the form of medication that could potentially offer these women the chance to witness their grandchildren grow and truly experience life. It is disheartening to note that only one Black patient was included in the clinical trial conducted for this medication. The remaining participants consisted of 96 individuals who are all White, two Asians, and two whose racial background is unknown.
Other Example again is a medication known as which is used for metastatic cervical cancer, which is prevalent in low and middle-income countries, particularly in Africa. However, in a specific clinical trial for this medication, only one Black patient was recruited, while the majority of participants were White. This lack of representation is a clear example of the inequity that exists in clinical trials. It is crucial that we address this issue and ensure that all individuals, regardless of race or ethnicity, have equal access to potentially life-saving treatments.
Inclusion in clinical trials is a topic that will be further discussed in an upcoming panel discussion. Before moving on to the questions, each participant was asked to briefly summarize what inclusion in cancer research and oncology means to them. For many, inclusion means that those who are most affected by the disease, such as patients themselves, should be actively involved in the research and have access to the benefits of scientific advancements. It is disheartening to see certain communities, particularly minority groups, being left behind in clinical trials. Representation and ensuring that those who bear the heaviest burden of a disease are included is essential.
Inclusion is not just a buzzword or a checkbox on a grant application. It requires genuine care and effort to design trials that address the needs of diverse populations. In a personal example, the speaker started a breast cancer support group in Abuja but recognized that as a non-survivor, she was not in the best position to lead it. True inclusion means empowering and supporting those directly affected by a disease to lead and guide initiatives. Unfortunately, inclusion often seems to only be prioritized when it directly affects those in power, as seen in the rapid development of a COVID vaccine compared to the lack of progress in addressing diseases like Lassa fever that primarily impact West Africa.
Moving on to the topic of making clinical trials more inclusive, it is acknowledged that one major challenge is the lack of access to trials for minority patients who do not receive their cancer care in big academic centers. Efforts should be made to bring trials closer to communities and improve accessibility. Additionally, the responsibility for inclusivity should lie with the researchers and providers, rather than solely on the patients. It is important to address biases and unconscious assumptions that may prevent certain individuals from being offered the opportunity to participate in trials. Compensation for trial participation should also be reevaluated to ensure that financial barriers, such as transportation costs, are not hindering participation.
In conclusion, achieving true inclusion in clinical trials requires a paradigm shift in the way trials are conducted and healthcare is delivered. It means treating everyone with equity, acknowledging that different individuals have different needs, and actively working to overcome barriers that prevent diverse populations from participating. By addressing these issues, we can work towards a more inclusive and equitable future in cancer research and oncology.So one of the trials I'm part of is a study led by Dr. Ky Doll, focused on social support for women with Endometrial Cancer undergoing adjuvant treatment. The study provides cell phones with data and compensation for participants. These strategies aim to improve enrollment. It's important to note that for many cancers, including blood and bone marrow cancers, gynecologic cancers, and prostate cancer, minorities often face disparities in diagnosis and treatment. Minorities are diagnosed at a younger age, which can create additional challenges such as needing time off work for clinical trial visits. This financial burden can deter participation.
During conferences, the issue of inequity in access to clinical trials is often raised. One common response is that there is a lack of infrastructure and clinical capacity. However, Africa, for example, is good for market access but lacks the necessary infrastructure for clinical research. This needs to be addressed in order to make progress in including ethnic minorities in clinical trials. Trust in local clinicians is also crucial, as they often have more experience with diverse forms of cancer than clinicians from high-income countries. Funding for global cancer research is also lacking in low and middle-income countries, which affects access to clinical trials and research in these areas.
Increasing representation in genomic studies faces similar challenges. Education plays a key role in ensuring understanding and acceptance of genomic studies. Explaining the purpose and aims of the study can help demystify genomics for participants. However, language barriers and cultural differences can impact communication and understanding. Tailored care and sensitivity to the experiences and concerns of different populations is necessary. Historical traumas and the loss of cultural identity can create hesitancy and a need for delicacy when discussing genetic research. The end goal of studying genomic diversity should always be precision medicine, as treatments may vary across populations.
In conclusion, addressing disparities in access to clinical trials and genomic studies requires improving infrastructure, building trust in local clinicians, and increasing funding for research. Education and tailored care are essential in ensuring understanding and acceptance among diverse populations.Oh, well, there has to be a biological basis and like, you know, it's just, it's just the genes, it's not just the genes, it's a society that's literally been built on the backs of people who have then been systemically disenfranchised to be further and further from healthcare. As they because of that distance from health care becomes sicker and sicker.
So the I guess I just wanna emphasize like, especially in conversations about genomic and biological DIVERSITY that the goal should be changing systems so that people have access earlier, access and consistent access to quality care, not so that we can point out all the things that are wrong and wrong in their genetics.
Absolutely. And just one Other point because we, we talk a lot about on the front end, how to recruit people in. on the back end, you have to take the data back to the communities because if you're building a relationship, so a lot of times people will just come in, take what they want, leave. It's important to circle back around and say this is what we found. This is what we learned and guess what that does. It creates a bond, it creates accountability. It shows that, you know, you're someone who, who cares about their input, their insights to, to tell them like this is what we found from you being a part of this, it creates a relationship. And guess what, you know, your, your next recruitment may go even faster. Because people know that this is how you work, this is how you operate and that you're not just gonna come grab what you want and leave.
So I think the feedback, the feedback loop, you know, like going back and telling them this is what we learned as a part of the Results. But also of the study would also be key. I, I just let me just let me just ask 222 seconds, two, I thought that just on that same Ben, I just wanna add something very important that I think you brought up.
I think it's important also to say that the family structure is really important as well. Which I think makes the genomic research a little bit different than clinical trials. And you say, well, what do I mean by that? What you can basically know is that you can say, hey, is this what they Call nature versus nurture? One of the big questions when we always talk about disparities and like, is there a difference in a group set in a set of people? Is, is this something that's biological or is this something that is due to a set of environment and what we Call SOCIOECONOMIC issues? And so I think that, you know, like you were saying that, that this would be a way that you can kind of take a minority group of people and say, hey, you know, we can look and see. Is this something that can affect your Children, your grandchildren? Is this something that was actually passed down to you? What do the actual breakdown of your cancer look like from a biologic standpoint? How aggressive is it? What are the features look like? You know, and I think that would be something because again, like I said, the family structure in minorities is something that's very held in high regard. And so I think that's something that would be very inst instrumental to kind of helping disseminate this type of research as opposed to others.
So sorry, sorry. No, no, no. You also made a very valuable point. Yeah, I just wanted to add to what Onya about you know, going back to the community, you know, we've also seen a lot of Experience of you know, helicopter research, you know, whereby you see people just have these very good projects and they just come down to maybe any middle income country, collect whatever data they want to collect and then they head off, that's it. And I would also say this is where I think publishers journals needs to have a role to play, you know, to ensure that when you're looking at me and you see where this data is coming from to also ask a question as an editor, right? This this data is coming from Africa. So why who are the authors? you know, II I mean, I'm currently, I'm currently, I'm currently working with a group of people on the Spirit and Consort Project, a very big Project. And the interesting thing we were saying is journal editors need to ask a question like, you know, this data is coming from Africa. Why is it that no African or even Africans Institution that is really in one of the authors? That's why you see many ARTICLES on different journals. These data were done in African genomic Project were done in different African. You see both the first author and all the Other authors are all from high-income countries. You will only see maybe one or two of one person from low income countries, they will just put the person in the middle and then you will see someone from high-income country getting citation of a Project in Africa. And you'll be seeing you'll be saying something like I don't want to use any name but maybe like a Pure American name at all on something that has to do with CULTURAL explanation or CULTURAL benefit, CULTURAL genomic science about specific type of cancer that affect this specific group.
So I think as much as we are also thinking global cancer control leaders to have a role to play, I think the journals also editors have a role to play and you know, this can we can I I think it's something that we can all do. It's just asking a very basic question and have them to include, include include you know, people from those, those community. I also just wanted to say something very quickly to say that currently in Nigeria, for instance, we have so many consortium that are doing genomic science projects we have because they don't really get the spotlight. So I wanna use the opportunity to spotlight them. We have for instance, a mayo clinic led Project by pro so for like your, you know, through doing millions of millions of projects which from ICA, one of them is called ICA. There's another one that is also called TC. Doing a lot of genomic science Project around prostate cancer. We also have Professor Lude, she's all doing a lot of projects around study and all the rest. So I want to say that many countries in Africa, many countries in Nigeria and many Lowerin countries are really ready. We Call the rest of scientists to really just reach out to people, reach out to advocates. They can really Help connect you to see how you can do this project. Nothing is no, is no longer impossible like as you were before. Yeah, so Runcie, you have hit on my next question exactly. Which was what can the publishers and also funding bodies be doing? Because, you know, we have a community in this Call today that has a lot of people that are within those communities. And as you say, we have a responsibility to ensure that these studies are done sensitively and, and also as Colon and an you both touched on the idea that these, these projects should be giving back to the communities that that research is being, being undertaken with.
So what do you think that we should be doing as a publishing community or funders, do you think that there are things that could be introduced to better ensure that research is inclusive and is inclusive of local researchers and is representative of the populations. I I think that, you know, one thing again, the research should typically reflect the population of people who are affected by the disease, you know, and so if you are, you know, run, you showed that that slide where it was like 1% you know, it was like, it was like one person, you know, it's like, come on, you know what I mean?
And so, and so, you know that as a high-quality journal, what we, what we expect is high quality science and we do know that from a high-quality science, we know that DIVERSITY is a AAA piece of that equation, right? And so not everybody is going to have DIVERSITY in their TRIALS, but maybe you could even have them put an explanation and say, hey, you know, we know that the incidence of minorities for this particular cancer is at 10%. But however, your trial only recruited 1%. Can you explain why? You know, and I think if you, you know, had people at least have but do an explanation. I think that we kind of gut check them a little bit to say like, oh man, the the publishers are, are, you know, they're asking for this, you know, like many of that like, you know, so like I'm sure you guys know this but like as you prepare to submit ARTICLES for the journals, you basically already know kind of what you expect them to ask if that makes sense and kind of what you know, you always, you come on like, you know, they typically there's so people that don't know when you submit for journals. Typically, what happens is that there's a revision process and then during that revision process, there's people who Review it and then they basically ask questions based off of the original manuscript that you submitted, but you kind of already have the answers to those questions that you already know that they're probably gonna ask ready so that it doesn't delay kind of the process.And so right now, if you say, hey, one of those questions that, you know, no one has asked you or that you're probably not prepared for is we've noticed this and what's up with that and what's, what's the reason for it? You know, then that way, you know, I, I think that really would be a big major step. You know what I mean? Not saying that people, you know, again, we will meet that bar but at least just have an explanation. Say, what, why did you fall short? You know, I think that would be a, a very good first step.
Yeah, I think that's a great Example of something that can be, you know, relatively simply included, but it's starting to get people to think about these questions and, you know, why, perhaps the, why is our population the way it is within this trial? because, because if you don't think about something, you won't make the change for it, right? Like, like if they're like, if you are able to, you know, do things the way that they've always been done and there's never been any checks or balances then it's like, why would you change it? Like, what do you mean? My, my papers get submitted and accepted all the time and, and that's just what, what happens we say, oh, there's a delay in my publication because of like, what is this happening? You, you know, or I have to give an explanation for what now, you know what I mean? And I, I think again, it's, it's literally just an explanation, like you're not asking them, you know, it's just like, well, we noticed this, what's, you know, what can you explain? Then? I think like I said, it would be a very reasonable thing that could be not a hard stop, but for sure, at least a yield, you know what I mean? Like a yellow light, traffic light, you know, just to say, hey, let's pay attention to this, you know, I think that that Brandon brings up a good point which is sometimes as we form and Investigate our research questions. We don't think about certain things as a community and we've never been, some folks have never been challenged to. And I don't necessarily I don't necessarily fault them for that. I don't, I don't believe in faulting individuals for systemic issues.
And so I think an easy adaptation, if you will from social science is just in biomedical science, we could adopt oppositionality statements. The term came from sociology. And essentially, if we just acknowledge that all parts of our identity are socially constructed and that identity influences the way that we look at the world, the way that we might ask and answer certain research questions. And for every publication that we wrote, we had to write a statement about how we position ourselves in relation to the research that we were doing. It might not even get to the point of a journal editor having to go. Hm I noticed this, it might be much, much earlier that someone goes hm, in thinking about like my identity in relation to this research, I realized that that connection is very Abstract. How might I bring in a collaborator? Even if it's all the way at the writing Stage to Help contextualize the Results in a way and it actually responsive to community. And so sometimes I feel like we get real deep into the weeds, like trying to reinvent the Wheel and these things already exist. It just sometimes haven't been adapted into our sector of science.
Thank you. Do you wanna add something or I should? Yes. Yes. I just wanted to add, you know, to the question that you said, what can you know, journals, you know, ask yourself can do I think first just to really appreciate Springer nature for hosting this conversation. I think this is the first step you've really done a very good job because you know, you know, Black researchers really need the voice, they need, you know, space to really share their passion and what you're doing right now. It's already phenomenal. We just need to build on it right now. So I think the next or what I think we could really do more is consider inviting more researchers from the Black communities to contribute to special issues. There are so many special issues out there that you know, they could contribute, even if to the basic minimum level of what is on ground, what is on ground can really Help us to appreciate what we already have. I was in a hospital in Tex and I had a patient who was really shouting and angry that she need. There's no co there is this very popular coffee shop in the radiation unit. She was really angry that the coffee shop was not there for her to have her coffee. And I looked at her, I was like, oh my God man back in Nigeria man, you wouldn't even, you know, you have to travel from here to like, you know, from take from Dallas to maybe like Houston like drive six hours, eight hours for you to have access to therapy. So when people in high-income countries see what's it's not a bili model settings, it helps them to appreciate what they have. People go crazy over Starbucks man. So yeah. No. Yeah. I didn't wanna mention the name. No, man. No. Listen, you can say it, man. Listen, if you don't have their coffee in the morning, it's a whole thing, man. Trust me. I understand. Listen, man. Hey, it's a problem I didn't wanna mention because I know the name but I didn't wanna mention I didn't wanna advertise yourself. Listen, you gotta let the truth out. Yeah. So we need to really invite the researchers from Black communities from Low and middle income countries. They may not give you all the big statistics or the big data, but you can tell at least what is going on the ground and what what would the FUTURE look like? I think Number two is journal and publishers can also do a lot in supporting these researchers. The truth is that most researchers from many Low and middle income countries from Black ethnic minorities are really ready to get improvement. They are really ready to learn because they've been through a lot, right? So understanding the fact that people are, people have been through a lot to pass through MB BS PhD post-doc. You know, all these challenges build up in social science. That is the theory known as cumulative inequality, the inequality people face at the younger Stage of their life as young researchers build up and contribute to what they could achieve at a later age. So this cumulative inequality Show the the disparity and capacity, the disparity in access to infrastructure, the disparity in how they Rise the disparity in the kind of information they could really pass on. But when journals begin to appreciate and understand that the Experience of these folks are different and their suffering, their struggles are different, you begin to appreciate where they are coming from.
And I think the last I would say is I, I think Jonah has a lot need to also do more in diversifying their editors, you know, when you diversify your editors and when I say diversification here, I mean, really not just inviting guest edits to sort of you know, Review or guest reviewers but diverse fine editors of different sessions, you know, think about sessions that I mean, I I know one and Doctor Blue and I think Kilan have also talked about when bo is highest in a particular group of people, why are we not facing, you know, imagine like cervical cancer, the the body all over the world. The greatest is where in Africa, you know, so think about those very innovative way to really include, include, include you know, Black researchers innovatively. And I just wanted to say this is also part of part of the work that we're doing with spirit and concert Team. And what we're saying is meaningful engagement of patients is the way to go. Now. It's no longer the days where we will just wanna include patient after we've gone like 70% of the entire process. I think that is also applicable to, you know, to publications, you know, having a way innovative way to also include patient to also include Black researchers. Thank you.
I also wanted to just add to that. Like I think something, you know, we talked about what journals can do. I would just caution to say something that I think they should avoid is kind of adding a like Black only Section. You know what I mean? Like sometimes like journals try to like make a special edition or a special collar. You know, like I think making it part of like nat like the normal jour like, you know what I mean? Like, it shouldn't be like only the people who have interest in this should care about this, you know, like this should be for everybody to read. And I think that's what sometimes happens is that II I, I'm not, maybe I'm not articulating it correctly but, but, but, but, but that I do see that sometimes and, and it hurts my Heart because that, you know, you're kind of preaching to the choir at that point. You know what I mean? Like, yeah, we all, we all on this Call may even know some of these things, but it's the Other readers who need to read about this.Those are the people who really, you know, we got to get the message out. And so I just caution against doing that if that was something that was on anybody's to do list for 2024.
I think you make some really, really important points there that we all, I think, should consider. But of course, as editors, if we look at clinical trials, they land on our desk when they are mostly done, but already in the design of clinical trials, I mean, what do you think is the role of funders or regulatory agencies?
So, you know, I'm sure you guys know about the FDA's what they call DIVERSITY plan, you know, as part of any drug that basically is going to get approved from the government. They have to have basically a DIVERSITY plan and how they plan to account for other groups of people. And I think that was a good first start, you know, that, you know, these companies are billion-dollar companies, you know, so they have resources. But are the resources going to the people who need them the most, you know. And so, you know, I think Runcie said an injustice anywhere is a threat to justice everywhere or something, you know, it was a good, like Martin Luther King kind of pivot he did. But, but I think that's what's needed, you know what I mean is that these companies that have money and have resources, they need to use that, you know, and so, I think that would be the best step.
So just quickly, Ony has just had to head off. She has another patient to see. But we just want to thank her for her time. So sorry to interrupt. Just wanted to say thanks for that. Ok. Any other thoughts about sort of the role of funding?
Yeah, I mean, I just, I just, I, I just want to add to what he says, you see the design of the study is so important. But I think to some level, there is really less of what journals can do when the data is already in your table just to review you see. Yes. Yeah. But I think what we need to really do a lot more is in terms of awareness creation, just to create awareness, to continue to create awareness, to really educate the clinicians. And I have worked with so many also clinicians from the US and also from Europe. And sometimes people miss this inclusion, not because they want to miss it, but it didn't occur to them. And I say this when I started, I said if something doesn't affect you, you don't think it's important, right? Yeah. So, but when we constantly create awareness, we will be getting closer to ensuring that designs replicate or designs really look at diversity and inclusion. Right? Yeah.
Absolutely. Well, I just wanted to change gear a little bit. We're coming towards the end of our time. But we've talked a lot about the patient experience and what I wanted to come round to is the topic of early career researchers and oncologists who are Black and they're sort of the challenges that might be faced. But Colon, I wanted to mention the stem Noir program is fantastic in terms of it's such a wonderful example of having a safe space for researchers across the stem sphere. And I know that we have some researchers here on this call. Now, I just wanted to ask, do any of you have advice or encouragement that you would like to give to Black early career researchers or later career researchers who are working within the oncology sphere.
I can keep it simple and quick. And I'll just share something that I wish someone had told me a little earlier on. Any environment where you don't feel as if you can be your full self, where you're having to make tradeoffs between who you are and what you do, is not the environment for you. Leave. For me, I would just say that any person who is a young investigator and trying to navigate their space in the world, it's important to build a team and don't be afraid of that team building being maybe not at your institution, you know. So, I hate to say this again, this is kind of to the choir but not everybody cares about improving the cancer disparity care. You know what I mean? Like that and, and if that's something that, you know, is part of your passion and that's your calling in the world is to research ways to make Cancer Care better for all groups of people that may not be everyone's and, and really may not even be a focus at your institution. But you can find that mentor, you can find that help, maybe even other places, but you need a team. And so I just would say, don't be afraid to build a team and, you know, especially, you know, with COVID and a lot of things being virtual and not, you know, as many people are meeting in person, use those resources available to meet up with someone out of a different institution and maybe be a part of your team to still be able to connect and still get, be successful with really the course that you plan to set for yourself. OK?
I would say one thing that has really been very that has really helped me a lot is building a community, right? And building a community is so powerful, especially if you are in your early career. The reason is that you need that community where you can always go back to really draw strength, sort of get inspiration, get motivated and also be able to loosen up and share your challenges. And so many Black and people from ethnic minorities who really in, in that, who are early investigators, probably in their post-doc level and all, and it's so difficult to really have that community. So that is really, really important. If you build that community, you would really, it would be easy for you to continue to navigate the system. The second thing I would also say is you know, find a mentor, right? But ensure that you find a mentor who is really interested in you and not just interested in what you bring in, you know, to the table. Because sometimes what I've seen sometimes is that many people have a lot that they want to really churn out in life, but they need someone that could help them to bring that peace out of them. So if you get a mentor that is just interested in what you bring to the table, that mentor will not be smart enough to really bring out that great things that you have in you that you can actually bring to the table. So these are my two, these are my 222 tips that has really helped me a lot in my career to really get work with mentors and build communities that really help me in the work that I do till today. OK?
I think we're slowly reaching the end of our time. So I just wanted to say that if anyone in the audience has any burning questions, now would be the time to still drop them in the chat. And I also wanted to say that if there is anything you still want to add, I think we still have a couple of minutes if you are, if there are any messages you want to get across, or maybe also, for example, to end on a positive note, if you want to share any examples of initiatives that you've recently gotten to know that you think have increased the inclusion in research and oncology. I would just say that for everyone listening, you know, we are here on this panel but we all needed help at some point, you know, we all have second guessed ourselves, you know, we all didn't know maybe what the future would hold. And so if you're at that point, if you're still kind of either in school or you're still kind of in a postdoc or, you know, still just trying to figure out life, that's OK. You know, and I just wanna be the first person to say that that it's ok to not have the next 10 years outlined, you know what I mean? But just, I think it's important to know is what fills your body with joy. You know what I mean? We only have one life to live and so you wanna make sure that you spend it doing something that fills your time with joy. I know that for me, I enjoy having these types of discussions. I enjoy helping patients who can't help themselves. I enjoy trying to research ways to improve blood and bone marrow. Like those are things that give me joy. And so you want to within yourself, take a deep dive and just kind of know what that is for you, which it's ok if it's not this like, like it's like, you know, like it's like we all have been there. But you wanna make sure that if you say that, hey, this is really what I enjoy that you wanna make sure that you don't get turned around and just know that there are resources out there to help you with whatever you're struggling with, whether that be funding there's resources, whether there is grant writing, you know, whatever it is that you think you might need help with, there's people out there that can help you.I appreciate everyone for listening and taking the time to listen. I want to encourage you all and hope that you have learned something today. Thank you, Doctor Blue, for your powerful words. For me, as a closing note, I want to emphasize that no matter what role we have in supporting cancer control, whether it's as a doctor, pathologist, clinician, psychologist, medical oncologist, editor, writer, or anything else, it's important to remember that we are all patients. The line between our specific roles and being a patient can change in an instant with a diagnosis. So it is important for all of us to work towards improving care and ensuring that people have another opportunity in life. Let's continue to raise our voices and create awareness, but let's not forget the power of advocacy in bringing about policy change. My vision is for the government to take over the work I am doing, so I will continue to raise my voice and advocate for their involvement. As we discuss raising awareness and including more Black researchers and clinical trials, we should also consider what policies we can create to ensure that diversity and inclusion are prioritized. We need practical solutions that will lead to sustainable change. The Black Lives Matter movement has shown that change is possible when we raise our voices, but we must also prioritize Black leadership. If you are a Black person listening to me, know that you have a role to play. Non-Black individuals can also contribute by raising their voices, providing support, and creating leadership opportunities. Thank you all for your time and for joining us today. We will take what we have learned into consideration. Thank you again to Doctor Blue and Kilan for participating.













































































![Runcie Chidebe
"A VERY PAINFUL JOURNEY"
"It's been a very painful journey, most especially when the
veins collapse
I suffer a lot, maybe because I'm big.
about nine pricks before I take chemo[therapy]. Nine full
pricks! [she exclaims] Every part of my hands [are]
vandalized
before I take chemo[therapy]
Because
knowing that I'm going to feel pain, I'm going to feel another
pain, more pain and still the result is not there [not successful]. In fact, it got to the point of using my leg and
still, it was still very difficult. I would say they [doctors] are
not patient
and not well trained. Their inpatient level can
lead you to develop cancer on its own."
www.projectpinkblue.org @projectpinkblue @runci](https://cassyni-user-files-prod.s3.amazonaws.com/Km1BCGtfhAb4KDB6KbjyM8)

![Runcie Chidebe
"TORMENTED BY PAIN"
"Ah! You don't wish the pain for your
enemy. / went through pain during the chemo[therapy] period / attempted suicide
because of pain The pain is second to
none. You cannot describe the pain; you don't know how to explain it. At a particular
time, you don't even know what is wrong
with you. Is it your stomach, your head, your
body? A pain you cannot describe"
www.projectpinkblue.org @projectpinkblue@runciecwo](https://cassyni-user-files-prod.s3.amazonaws.com/LFenExYC8d9CfRERkEpEAz)





